SLAP lesions
SLAP lesions were not recognized until the 1980’s when keyhole surgery of the shoulder was starting to be performed. SLAP stands for superior labrum anterior and posterior, which defines the anatomical location of the injured area.
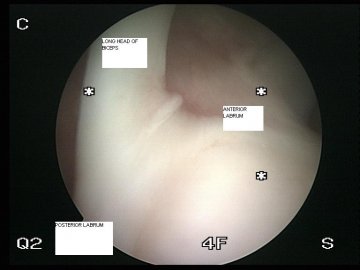
The tendon of the long head of biceps enters the shoulder and runs within the shoulder joint to its attachment at the superior part of the glenoid. Here it joins the labrum which runs both anterior and posterior around the glenoid.
A normal biceps attachment is shown below
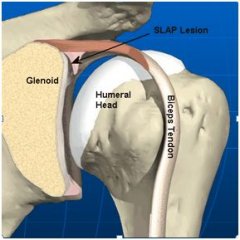
This attachment of the biceps can be injured and this is when we get a SLAP lesion.
This diagram shows the biceps and its detachment in the socket
How does injury occur?
There are two main ways of injury, through repetitive overhead use or through isolated traumatic events.
Trauma include collisions, fall onto outstretched arm wrenching away from the body. SLAP lesions can also occur with dislocations of the shoulder. Repetitive injury occurs with overhead activity in throwing sports, racquet sports and swimming.
Classification of injury
A classification of SLAP lesions was devised by Synder in 1990 with types I-IV.
- Type I – fraying at the edge of the labrum
- Type II – detachment of the biceps anchor from the glenoid
- Type III – bucket handle tear of the labrum
- Type IV – the tear extends up into the biceps tendon
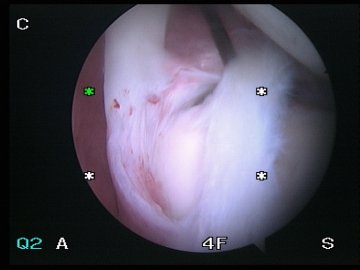
This is an example of a Type III SLAP lesion
Symptoms
Can often be vague with deep pain within the shoulder, pain can occur with overhead activities and be confused with impingement. There may be a lack of ability to return to the same level of sport and/or overhead activities. Patients can experience a clicking or clunking within the shoulder and often describe a lack of trust in the shoulder.
Diagnosis
There are a number of clinical teats described to assess SLAP lesions, but none are accurate enough to be useful in isolation. MRI arthrogram can be used to aid diagnosis and will show contrast getting under the edge of the torn labrum. The reported accuracy of this is about 70-80% of cases.
Treatment
Treatment is dependent on symptoms, as some older patient’s with lower physical demands may not have significant problems. However in the symptomatic young athlete arthroscopic repair is recommended.
Arthroscopic assessment of the SLAP lesion allows decision making to confirm the diagnosis. The decision to repair a SLAP lesion depends on the findings, if the biceps is unstable and there is fraying of insertion and damage to edge of articular cartilage of the socket then repair is indicated.
The labrum is reattached to edge of the socket with aid of suture anchors. These are devices which attach to the bone allowing sutures to be passed through the biceps anchor allowing this to be reattached. This gives a temporary hold until the biological bond is restored.
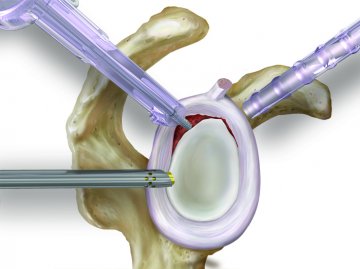

The diagrams depict a SLAP lesion being repaired arthroscopically.
Postoperatively a sling is worn and pendular exercises are performed to keep the shoulder mobile. Progression to active assist exercises usually occurs at about 4 weeks.
Andrew Brooksbank

CONSULTING HOURS
CONTACT DETAILS
CONDITIONS
Treatment journey
APPOINTMENTS
Make a consultantion appointment wiith Mr Andrew Brooksbank at BMI Ross Hall Glasgow.
FAQ’s
Frequently asked questions about appointments, treatment, recovery and insurance/payments.

